Cracking down on Hepatitis C in Indigenous communities
- embody
- Jun 16, 2018
- 2 min read
Updated: Sep 12, 2018
by Rayane Tamer |

A state-wide intervention program hopes to knuckle down the rising climb of Hepatitis C in Indigenous communities.
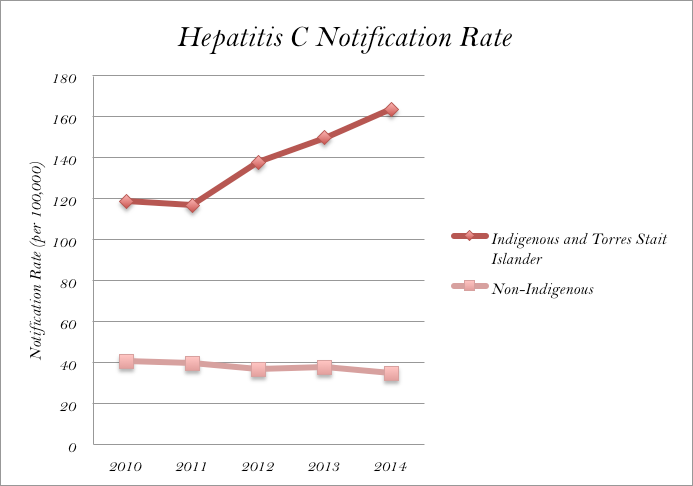
The Deadly Liver Mob project is tackling the “alarming figures” that indicate Indigenous people are up to eight times more likely to contract Hepatitis C than non-Indigenous people.
UNSW Director of Social Research in Health, Carla Treloar, saw the program boost access to sexual health services for the community by 1023 per cent per annum since 2013, and has since rolled out across seven local health districts (LHDs) around NSW.
“The Aboriginal community, like with many health conditions, bears the burden of Hepatitis C, so the importance of engaging the community with education is paramount,” Ms Treloar said.
"It feels as though the government doesn’t care because they don’t.”
The program has an incentive for the Indigenous community too, with clients receiving $20 supermarket vouchers by participating in their initial education course.

While Ms Treloar says the vouchers ensure positive engagement with the community, Indigenous activist Gavin Stanbrook believes otherwise.
“Some people can think it’s racist. Like, ‘what are you saying? We’ve all got gonorrhoea?’” Stanbrook said.
The Gumbaynggirr countryman acknowledges the program to be “positive and meaningful”, but he believes it is the responsibility of the government to do more in order for change to happen.
“Racism is the vehicle by which Aboriginal communities are othered and subjected to this level of neglect. It feels as though the government doesn’t care because they don’t.”
Statistician on Indigenous affairs, Professor Richard Madden, said that while there is funding for the figures, the problems found from the figures remain unsolved.
“Whether there is enough money from the government is the problem, and you can’t convince them to start programs,” he said.
With the notification rates of Hepatitis C increasing in Indigenous communities, yet decreasing in non-Indigenous populations, it is difficult for people like Karen Beetson to trust that there will be any systematic progress.
Ms Beetson, the deputy director of Aboriginal health in south-western LHDs, said that the Deadly Liver Mob project is not a realistic tool to combat the communicable disease.
“I don’t think this program is sustainable because I don’t believe the government will put in a long-term plan,” she said.
“We can’t just have one program… we need a national campaign that gets people talking the same language for Aboriginal health.”
Meanwhile, Professor Madden remains positive that if “you speak loud enough, you will get a response.”
The Deadly Liver Mob Project was established in Western Sydney LHDs, where it saw 400 Indigenous people engaging in health care activities in the first 12 months.






Comments